Hi friends! I’m back with a new blog post (albeit wayyy later in the day), and for this one, I’m talking about pregnancy and infant loss—a topic I know all too well. So much of what’s out there describes what not to do or say to someone who has experienced this type of loss. Of course, this is crucial, but we also need to provide people with the information, tools, and support of what to do.
Before we get started, let’s go over some basic terminology and general statistics (note, these statistics are taken from PSI–Postpartum Support International):
A miscarriage is a loss that occurs at up to 20 weeks gestation, while a stillbirth is classified as a loss beyond 20 weeks gestation. Pregnancy and infant loss are not uncommon. These statistics clearly speak to its prevalence—1 in 4 known pregnancies will end in loss.
We know that loss is more likely to occur in the 1st trimester (80%), less likely to occur in the 2nd trimester (14%) and even further likely to occur in the 3rd trimester (6%). These statistics lead to a false sense of security that our society fosters—the notion that if a woman makes it to the 2nd trimester, she is in the “safe zone” of pregnancy, when in reality, there is no such thing as a true safe zone. These statistics also don’t account for other types of loss such as TFMR (termination for medical reasons), a loss during childbirth, or a loss shortly after birth. When I write or speak about loss, I use this as an umbrella, all-encompassing term for all types of pregnancy and infant loss. Each type of loss is extremely nuanced, and all are deeply and profoundly painful.
Pregnancy and infant loss are not uncommon, yet these experiences of loss and grief are too deeply personal and profoundly impactful to stop at acknowledging how common they are. So, we know loss is common. But what we don’t know—or rather, what we tend to talk about less frequently, is how to support someone who has experienced a loss.
Instead, we try to “fix” the problems or cure them of their grief. Though typically well-intended, this only creates a further divide. It prevents those who are grieving a pregnancy/infant loss from accessing the support they so desperately need, and it leads those who are trying to support a loved one, to feel helpless.
One of the most important things to realize is that there is no remedy for grief. There is nothing that can be done or said to help someone “snap out” of their grief. As much as we’d like to believe that there is a solution to everything, some things just simply cannot be fixed—and that’s ok.
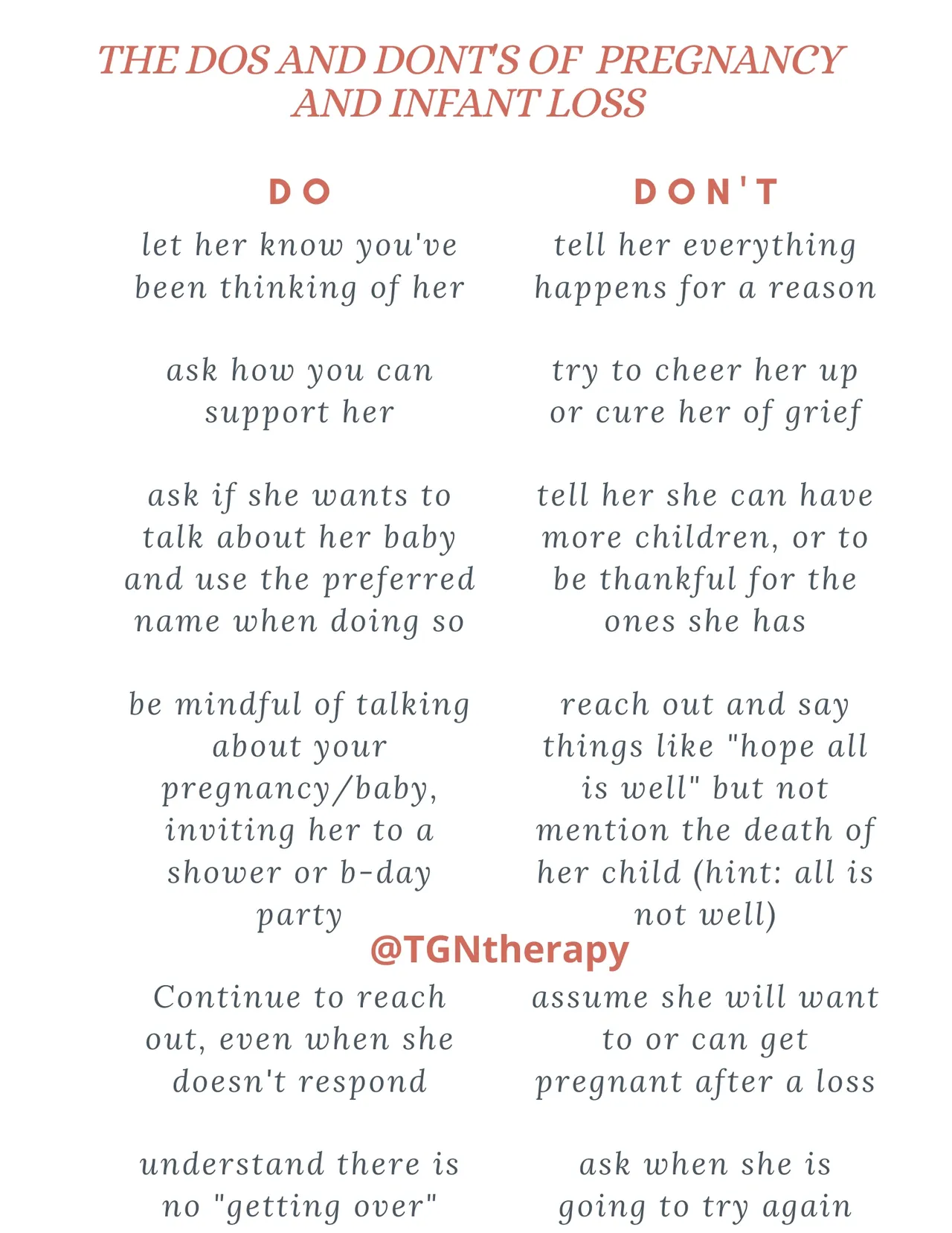
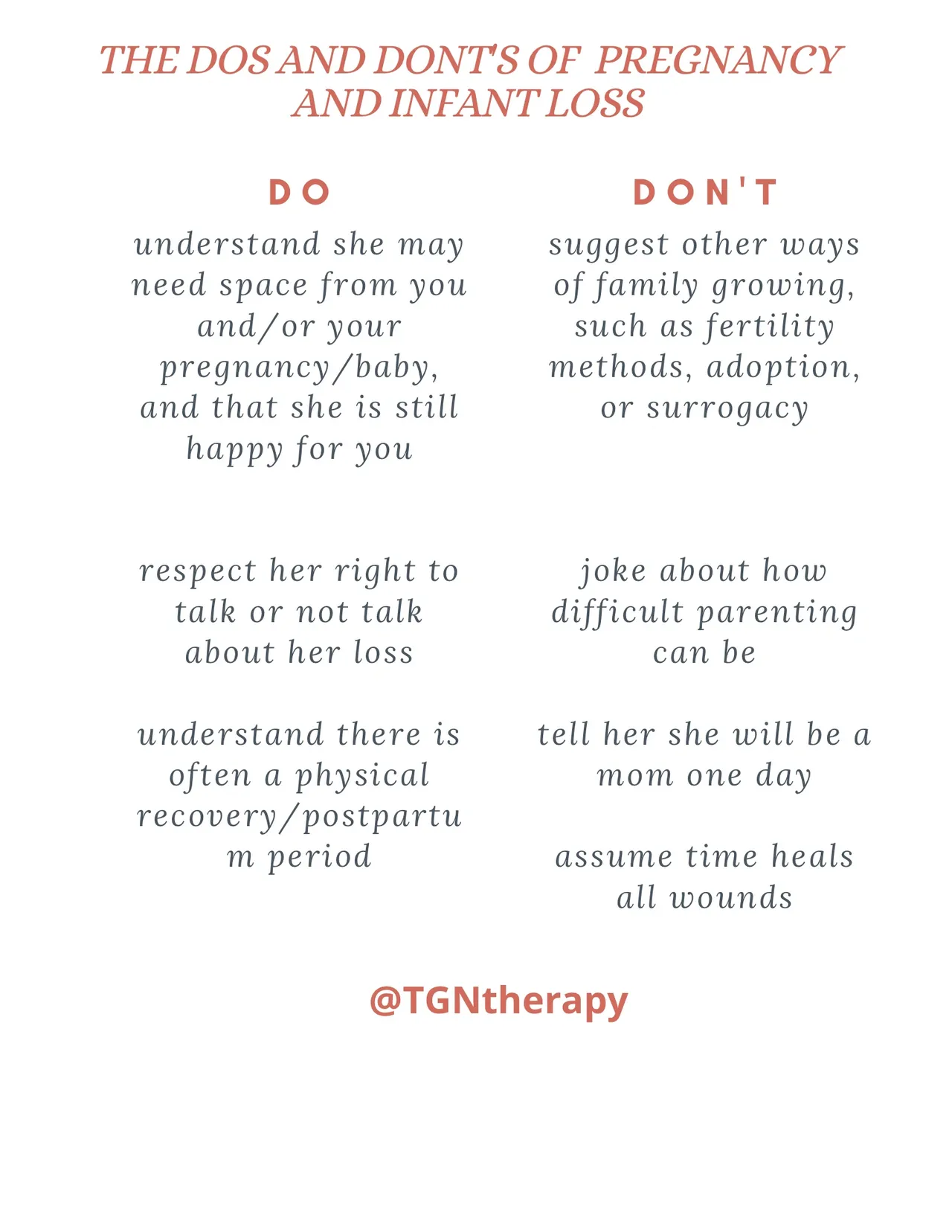
In an effort to help advocate for appropriate support of women and families who find themselves on the heartbreaking side of these statistics, here is a cheat sheet of some common dos and don’ts related to pregnancy and infant loss.
Please note: the best way to know what someone needs, is to ask them directly. Needs may differ, and whatever your/their needs are—they are valid.
This list is based off of my personal experience (I’ve had a 3rd trimester and 1st trimester loss), my professional experience as a therapist working in this space, and that of many within this community.
There is a common misconception when it comes to supporting those who have experienced this type of loss: if I talk about what has happened to them, I will make them sad. This is just simply not true. They are sad and not only is this to be expected—this should be accepted.
People who are grieving desire to be in the company of those who get it. They want to be around others who don’t shame them for normative expressions of grief. They want to spend time with someone who will not cringe at their dark humor, “negative expressions,” or feel uncomfortable when they cry.
There is nothing you can do or say to take their pain away, but what you can do is sit alongside them in it. And that, my friends, is the most valuable thing you can offer a grieving person, for there is no greater gift to a grieving loved one, than a witness.
For more articles on how to support those who have experienced pregnancy or infant loss, follow us on Instagram (@TGNtherapy), check out our other blog posts, and click here for additional perinatal resources.
by: Tracy Gilmour-Nimoy, M.S., LMFT, PMH-C